Abstract
Background: Despite significant advances in cardiovascular care, smoking remains a critical risk factor for recurrent cardiovascular events in myocardial infarction (MI) survivors. Primary percutaneous coronary intervention (PCI) is a lifesaving procedure; however, its long-term success is often compromised by patients’ continued smoking.
Objective: This qualitative study aims to explore the experiences, perceptions, and barriers faced by individuals who continue smoking after undergoing primary PCI for MI, providing insights into the psychological, social, and behavioral factors that hinder smoking cessation.
Methods: A qualitative research design was adopted, involving semi-structured interviews with post-MI patients who continued smoking. Thematic analysis was employed to identify and interpret key themes related to smoking behaviors, challenges in quitting, and the effectiveness of current cessation interventions.
Results: Participants acknowledged the health risks of smoking, linking it to their MI, yet highlighted significant barriers to cessation, including stress management, emotional reliance on smoking, and ingrained habits. Social influences and cultural norms were also contributing factors. While healthcare professionals provided critical advice, participants reported limited success with available cessation methods, emphasizing the need for comprehensive, personalized support.
Conclusions: Smoking cessation remains a significant challenge for post-MI patients, driven by a complex interplay of addiction, emotional dependence, and social influences. Effective interventions should incorporate stress management, tailored support systems, and innovative cessation tools to address these barriers. Promoting smoking cessation is essential to enhancing the long-term outcomes of PCI and reducing cardiovascular risks. Further research should focus on scalable, patient-centered approaches to empower MI survivors in overcoming smoking addiction.
Keywords: acute myocardial infarction, percutaneous coronary intervention, smoking cessation
Introduction
Despite significant advances in cardiovascular treatment, smoking remains a persistent risk factor for myocardial infarction (MI).1-3 Primary percutaneous coronary intervention (PCI) is a lifesaving procedure that restores blood flow to the heart during acute MI.4 However, the success of PCI in prolonging life and improving outcomes can be undermined by continued smoking.5,6 Smoking cessation is critical after MI, as it reduces the risk of recurrent cardiovascular events and mortality.7,8 Yet, many patients struggle to quit smoking even after a life-threatening event such as MI9. Understanding the underlying reasons behind this challenge is vital for designing effective interventions.9,10
This qualitative study focuses on individuals who have undergone primary PCI following MI but continue smoking. By exploring their experiences, perceptions, and barriers to cessation, this research aims to shed light on the complex interplay of psychological, social, and behavioral factors that perpetuate smoking despite significant health risks.
Methodology
Study design
The study included five participants presenting to the outpatient cardiology clinic at Ankara Bilkent City Hospital with varied demographic profiles: a 62-year-old male, a 45-year-old female, a 54-year-old male, a 39-year-old female, and a 68-year-old male. Ages ranged from 39 to 68 years, with two females and three males. Smoking behaviors were influenced by stress, emotional dependence, and social norms across all participants.This study employed a qualitative research design to explore the experiences and perspectives of individuals who continued smoking after experiencing a heart attack. Semi-structured interviews were conducted to obtain rich, detailed data about the participants’ smoking habits, attempts to quit, and the barriers they faced. Thematic analysis was used to identify and categorize recurring patterns and themes.
The study included five participants who met the following inclusion criteria: to ensure confidentiality, participants were anonymized and labeled as K1 to K5.they were 18 years of age or older, had been diagnosed with myocardial infarction within the past two years, were actively smoking at the time of the study, and were able to provide informed consent and participate in interviews conducted in Turkish.
Data were collected through in-depth, semi-structured interviews conducted either in person or via secure video conferencing platforms. An interview guide was developed to ensure consistency while allowing flexibility to explore individual experiences. Key areas of focus included:
- Smoking history and reasons for initiation.
- Past attempts and motivations to quit smoking.
- Perceived health risks and advice from healthcare professionals.
- Emotional and social factors influencing smoking behaviors.
Each interview lasted approximately 30-45 minutes and was audio-recorded with participants’ consent. Field notes were taken to capture non-verbal cues and contextual observations.
The audio recordings were transcribed verbatim, and transcripts were analyzed using Braun and Clarke’s thematic analysis approach: (Table 1)
| Table 1. This table presents the codes generated from the analysis of participant statements and the themes derived from these codes | ||||||
| Theme | Code |
|
|
|
|
|
| Smoking Initiation | Peer Influence |
|
||||
| Stress Relief |
|
|
||||
| Role Models |
|
|||||
| Social Norms |
|
|||||
| Rite of Passage |
|
|||||
| Challenges in Quitting | Cravings |
|
||||
| Stress/Addiction |
|
|
|
|
||
| Emotional Crutch |
|
|
||||
| Perception of Harm | Acknowledgement of Harm |
|
|
|
|
|
| Heart Attack as Wake-Up |
|
|||||
| Role of Doctors | Advised to Quit |
|
|
|
|
|
| Emotional Impact | Guilt |
|
||||
| Shame |
|
|
||||
| Resignation |
|
|||||
- Familiarization with the data through repeated reading.
- Initial coding to identify key phrases and concepts.
- Grouping codes into broader themes reflecting shared experiences.
- Refining and defining themes to capture the essence of participants’ perspectives.
MAXQDA 2023 software was used to facilitate coding and visualization of the data. A secondary coder reviewed the transcripts to ensure consistency and reliability of the themes.
Ethical approval for the study was obtained from Ankara Bilkent City Hospital Ethics Committee TABED 2-24-08. Informed consent was obtained from all participants prior to data collection. Participants were assured of confidentiality, and identifying information was anonymized in the transcripts and analysis. They were also informed of their right to withdraw from the study at any time without any consequences.
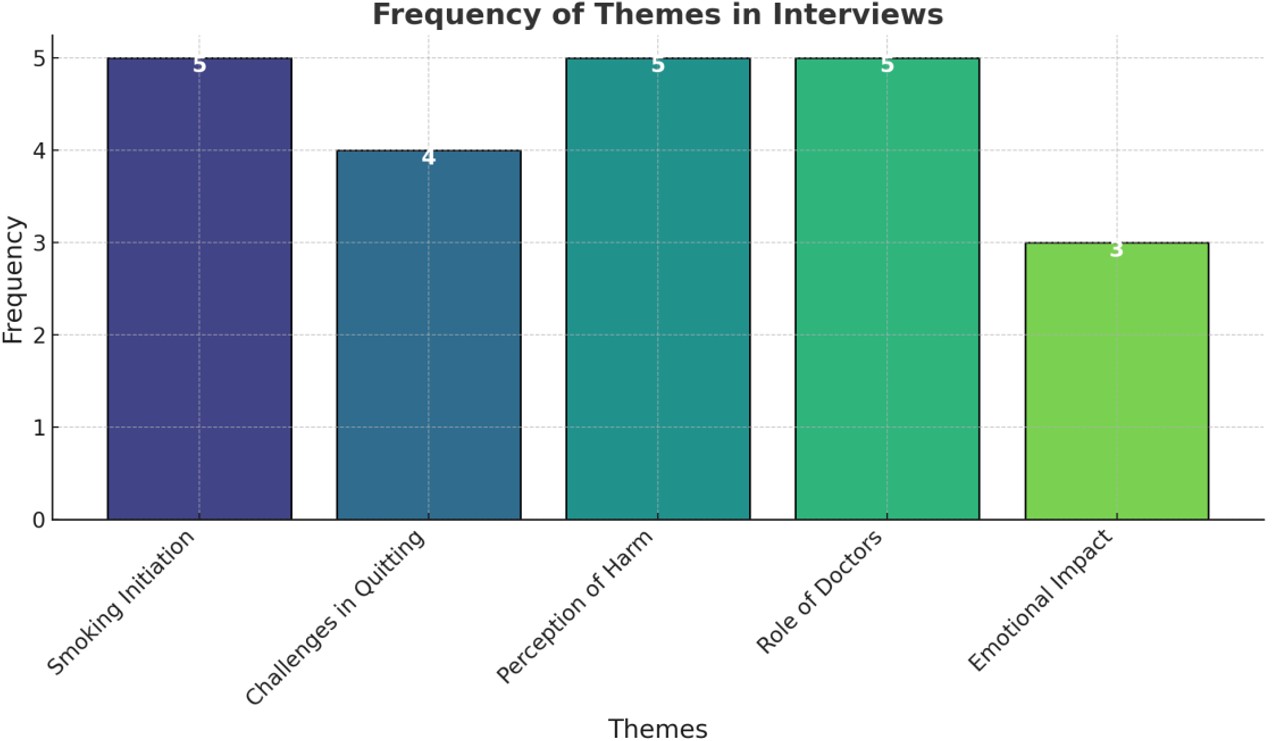
This methodology ensures rigor and transparency in exploring the complex interplay of psychological, social, and health-related factors influencing smoking behavior post-myocardial infarction (Figure 1).
- Identify and code themes or categories in the interviews.
- Organize codes into broader categories or “parent themes.”
- Provide an example summary of insights based on the analysis.
Step 1: Initial Coding
1. Smoking Initiation
- Peer Influence: “Most of my friends smoked” ( K4).
- Stress Relief: “It helped me stay awake during long shifts” ( K1 ).
- Role Models: “My older sister smoked, and I wanted to be like her” ( K3 ).
- Social Norms: “It was common in my social circle” ( K2).
- Rite of Passage: “It felt like a rite of passage in the police academy” ( K4).
2. Attempts to Quit Smoking
- Multiple Attempts: “I’ve tried several times” ( K3).
- Temporary Success: “I managed three months but started again after a stressful day” (K1).
- Methods Tried:
- Nicotine Replacement: “I tried nicotine gum and patches” (K4, K1).
- Alternative Therapies: “I tried acupuncture” ( K2 ).
- Digital Tools: “I used a smoking cessation app” ( K3).
3. Barriers to Quitting
- Stress and Addiction: “Running my business is stressful, and smoking helps me think” (K2).
- Emotional Crutch: “Smoking feels like my comfort zone” ( K3 ).
- Cravings: “The cravings were unbearable” (K5).
- Habits: “It’s a habit I’ve carried for decades” (K4).
4. Perception of Smoking’s Harm
- Acknowledgement of Harm: All participants recognized smoking as harmful: “Of course, I know it’s bad” ( K5).
- Heart Attack as a Wake-Up Call: “I blame myself for the heart attack” (K5).
- Conflicted Feelings: “I feel ashamed, but I also feel overwhelmed” (K1).
5. Role of Healthcare Professionals
- Advised to Quit: All participants reported being advised to quit by doctors.
- Support Offered: “He suggested counseling” (K5).
- Firm Guidance: “My cardiologist was very firm about it” (K1).
6. Emotional Response to Smoking
- Guilt: “I feel guilty, especially when my family brings it up” (K5).
- Shame: “It’s embarrassing because I know better” (K1).
- Resignation: “I feel disappointed in myself but also resigned” (K4).
Step 2: Broader Themes
The codes are grouped into the following broader themes:
1. Social and Psychological Origins of Smoking
- Peer influence, stress, role models, and social norms.
2. Challenges in Smoking Cessation
- Cravings, emotional dependence, stress, and deeply ingrained habits.
3. Health Awareness and Doctor’s Role
- Perception of harm, wake-up calls, and doctor-led interventions.
4. Emotional Impact of Smoking
- Guilt, shame, and resignation.
5. Interventions and Coping Strategies
- Nicotine replacement, alternative therapies, and digital tools.
Step 3: Insights and Patterns
Based on the analysis:
Commonalities Across Participants
- All participants are aware of smoking’s harmful effects, particularly after their heart attack.
- Stress and addiction are significant barriers to quitting for all interviewees.
- Healthcare professionals play an essential role in raising awareness but are often not enough to ensure cessation.
Differences Among Participants
- Motivation to Quit: K3 and K1 show more willingness to try various quitting methods, whereas K4 appears resigned to his habits.
- Triggers for Initiation: Social influence dominated younger smokers’ initiation (e.g., K3 ), while stress was a key factor for others (e.g., K1, K2).
This study reveals that smoking cessation remains a significant challenge for heart attack survivors due to stress, ingrained habits, and psychological dependence. While healthcare professionals provide critical advice, participants often lack sustained support to quit. Future interventions should target stress management, provide comprehensive support systems, and address the emotional aspects of quitting.
Discussion
The findings of this study reveal a multifaceted struggle among post-MI patients to quit smoking, highlighting the interplay between addiction, emotional dependence, and social influences. Participants consistently recognized the harmful effects of smoking, often associating it with their heart attack. Despite this awareness, deeply ingrained habits, stress management, and emotional reliance on smoking emerged as critical barriers.
Many participants cited stress as a primary trigger, describing smoking as a coping mechanism for emotional and situational challenges. This aligns with existing literature, which suggests that stress and addiction are significant obstacles to smoking cessation in cardiac patients. Additionally, social and cultural norms surrounding smoking during formative years played a role in initiating and sustaining the habit.
The role of healthcare professionals was acknowledged by all participants. Doctors’ advice to quit was often perceived as firm but insufficient in addressing the complexity of their addiction.11 While participants expressed a desire to quit, they reported limited success with available cessation methods, such as nicotine replacement therapy or behavioral counseling. This suggests a need for tailored, multifaceted cessation programs that address both the psychological and social dimensions of smoking.
Moreover, this study did not investigate whether participants sought or received professional support for smoking cessation. This is a notable limitation, as the literature clearly demonstrates that structured interventions combining pharmacotherapy and behavioral therapy significantly improve quit rates among cardiac patients.12 Including this dimension in future research would provide a more comprehensive understanding of barriers and facilitators to cessation.
Additionally, the small sample size is a limitation that should be explicitly acknowledged. While qualitative research allows for in-depth exploration, broader studies with larger, more diverse populations are necessary to enhance the transferability of findings.
Several national studies, including research conducted in Türkiye, have also emphasized the importance of long-term follow-up, emotional support, and accessibility of cessation services in ensuring sustained abstinence among post-MI patients.13 Incorporating such data would have further enriched the analysis.
Conclusion
This study underscores the difficulty of quitting smoking among post-MI patients, even after primary PCI. The findings suggest that while awareness of the risks is high, stress, emotional dependence, and ingrained habits create substantial barriers to cessation. Effective interventions should go beyond medical advice, incorporating stress management strategies, personalized support systems, and innovative cessation tools to address the complex needs of this population.
In light of these findings, it is essential to develop integrated cessation programs that combine medical, psychological, and social support to meet the unique needs of cardiac patients.
Promoting smoking cessation in post-MI patients is not merely a recommendation but an urgent necessity to enhance the long-term success of PCI and improve overall cardiovascular outcomes. Further research is needed to explore scalable, patient-centered approaches that empower individuals to overcome addiction and embrace healthier lifestyles.
Ethical approval
This study has been approved by the Ankara Bilkent City Hospital Ethics Committee (approval date: 15.05.2024, number: TABED 2-24-08). Written informed consent was obtained from the participants.
Source of funding
The author declare the study received no funding.
Conflict of interest
The author declare that there is no conflict of interest.
References
- Zaheen M, Pender P, Dang QM, et al. Myocardial infarction in the young: aetiology, emerging risk factors, and the role of novel biomarkers. J Cardiovasc Dev Dis 2025; 12: 148. https://doi.org/10.3390/jcdd12040148
- van Berkel TF, van der Vlugt MJ, Boersma H. Characteristics of smokers and long-term changes in smoking behavior in consecutive patients with myocardial infarction. Prev Med 2000; 31: 732-741. https://doi.org/10.1006/pmed.2000.0755
- Rallidis LS, Hamodraka ES, Foulidis VO, Pavlakis GP. Persistent smokers after myocardial infarction: a group that requires special attention. Int J Cardiol 2005; 100: 241-245. https://doi.org/10.1016/j.ijcard.2004.08.040
- Abubakar M, Javed I, Rasool HF, et al. Advancements in percutaneous coronary intervention techniques: a comprehensive literature review of mixed studies and practice guidelines. Cureus 2023; 15: e41311. https://doi.org/10.7759/cureus.41311
- Hasdai D, Garratt KN, Grill DE, Lerman A, Holmes DR. Effect of smoking status on the long-term outcome after successful percutaneous coronary revascularization. N Engl J Med 1997; 336: 755-761. https://doi.org/10.1056/NEJM199703133361103
- Ashby DT, Dangas G, Mehran R, et al. Comparison of one-year outcomes after percutaneous coronary intervention among current smokers, ex-smokers, and nonsmokers. Am J Cardiol 2002; 89: 221-224. https://doi.org/10.1016/s0002-9149(01)02205-6
- Saxena A, Shan L, Reid C, et al. Impact of smoking status on early and late outcomes after isolated coronary artery bypass graft surgery. J Cardiol 2013; 61: 336-341. https://doi.org/10.1016/j.jjcc.2013.01.002
- Zhang YJ, Iqbal J, van Klaveren D, et al. Smoking is associated with adverse clinical outcomes in patients undergoing revascularization with PCI or CABG: the SYNTAX trial at 5-year follow-up. J Am Coll Cardiol 2015; 65: 1107-1115. https://doi.org/10.1016/j.jacc.2015.01.014
- Koçak A, Yıldırım O, Coşgun A, Türkkanı MH. Factors affecting smoking cessation after acute myocardial infarction. Thorac Res Pract 2023; 24: 151-156. https://doi.org/10.5152/ThoracResPract.2023.22139
- United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the surgeon general. Washington (DC): US Department of Health and Human Services; 2020.
- Rigotti NA, Munafo MR, Murphy MRG, Stead LF, Munafo MR. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev 2002. https://doi.org/10.1002/14651858.CD001837
- Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev 2013; 2013: CD009329. https://doi.org/10.1002/14651858.CD009329.pub2
- Demir Alsancak A, Şengezer T, Alsancak Y et al. Akut koroner sendromların sigara içme davranışları üzerine kısa ve orta vadeli etkileri, taburculuk sonrası sigara içme durumunu etkileyen faktörler ve aile hekimlerinin rolü. Istanbul Med J 2020; 21: 443-450. https://doi.org/10.4274/imj.galenos.2020.70457
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.